Dementia and podiatry can be a complex combination. It may not be the first thing you think about, but did you know that podiatry is an extremely important part of dementia care? People with dementia can be prone to loss of sensitivity and padding in their feet and can also be affected by collapsed arches or poor blood circulation. Read on to learn how Podiatrists support those living with dementia within home and aged care during treatment interactions by using effective communication, being patient, and limiting distraction.
Podiatrists can assist in helping to manage and offset many of the neuro-biomechanical effects of dementia, working to aid balance and awareness to maximise the functional range of motion to keep individuals active. Podiatrists are also the clinicians tasked with managing skin and nail health for the lower limb. In many ways this is very basic podiatry; it represents a narrow scope of practice. However, it is vital to injury and disease prevention but becomes complex when cognition is impacted.
What is the role of a Podiatrist and how do they treat individuals with dementia?
Our Podiatrists must be patient, reassuring, and adapt to their client’s needs. A Podiatrist’s presence and treatment can often be overwhelming and intimidating, because of the tools used during intervention. While many of the strategies our podiatry team use in this process are widely used by all allied health services, others are unique as often Podiatrists need to work efficiently, communicate effectively, and take care not to negatively stimulate the client. Some of the strategies include:
- Engaging with nursing and care staff within aged care environments to support and mobilise residents. These teams are very familiar to clients and can often aid communication and provide reassurance to the resident.
- Request staff or family to be present for treatment to provide reassurance, translate for the resident, or provide distraction. It is important that anyone present during the treatment be a calming influence to avoid podiatry accidents.
- Utilise behavioural therapy aids such as comfort objects or background music.
- Utilise a private treatment space for the residents to visit, rather than requiring them to return to their rooms. Often asking someone to return to their room for treatment can lead to distrust of the clinician; as a result, using a space that is neutral, calm and inviting can help.
- Speaking calmly, clearly, and in a friendly but non-patronising tone. Take care to avoid complex instructions and moderate volume, as this can often confuse and overstimulate individuals.
- Pause to observe, palpate, then treat. By looking at the feet first, the podiatrist can essentially triage the treatment needs.
- Work as efficiently and conservatively as possible, remembering that the aim of treatment is to provide preventative care.
It is vital that at all times the client’s dignity and choice be respected, if they do not consent to care or withdraw consent, treatment should not go ahead. The Podiatrist should then speak with the nurse on duty, who may follow up with the resident and the treatment be done later, or ensure that the choice not to receive care is documented.
A Real Life Case
One of our Podiatrists recently encountered a complex situation regarding consent with an individual with dementia at a residential aged care facility. The clinical manager asked the Podiatrist to review a resident, as the resident’s son had notified staff that his father’s toenails had not been treated recently. Unfortunately, this was due to the resident having a history of complex behavioural patterns, and despite the care staff’s best efforts, treatment could not previously be completed.
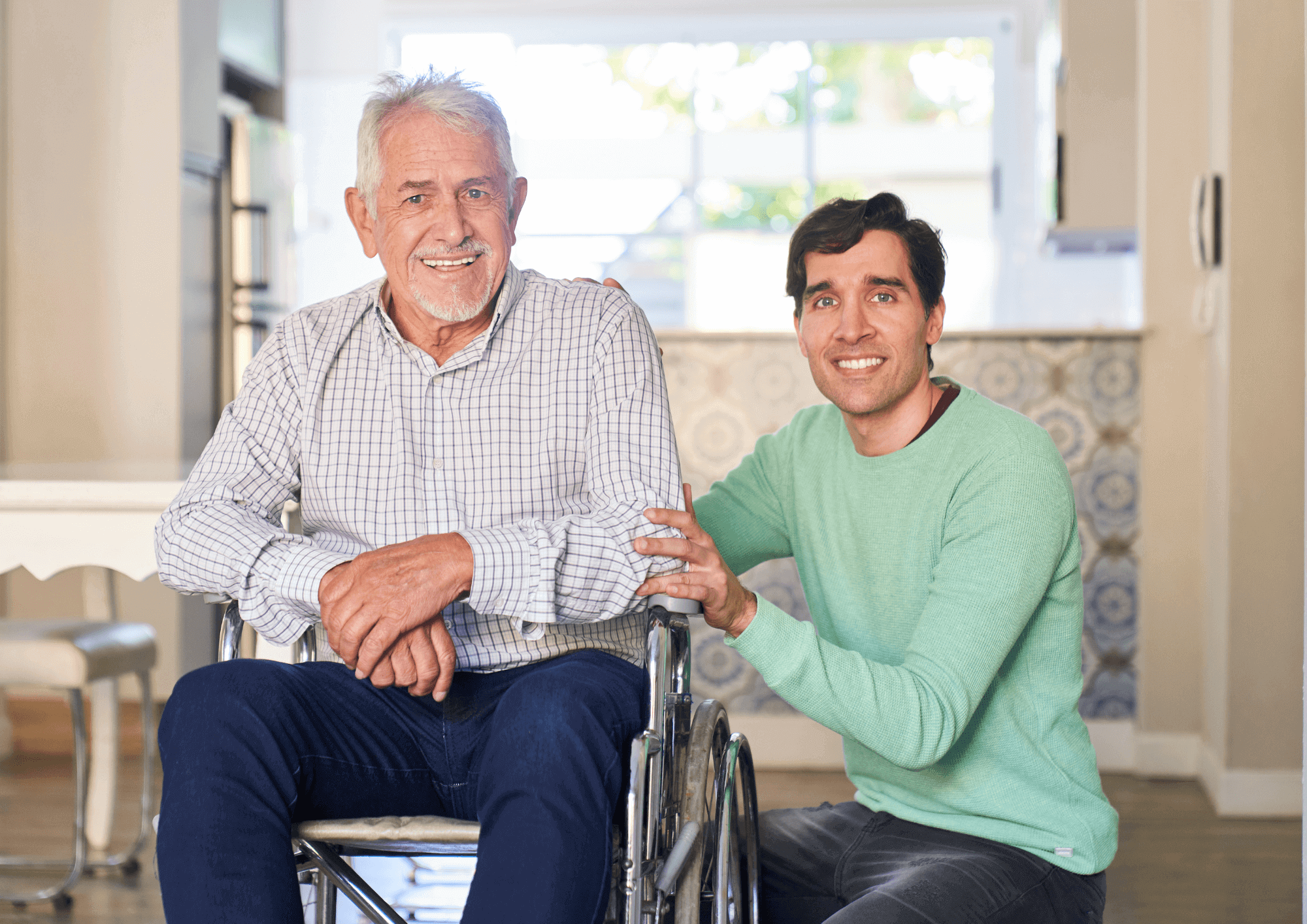
The resident’s son suggested that their father should be physically restrained for treatment if necessary. This contravenes both Plena’s practices and AHPRA consent guidelines, and the son was informed of this. Our Podiatrist advised they would attempt treatment but would have to stop if the resident withdrew their consent. Unfortunately, treatment was not possible and was deferred to the following day when the resident’s son could be present. Our Podiatrist spoke with the resident’s son before treatment and suggested a new plan. If he was comfortable, providing reassurance and distraction to his father would be very helpful. As a result, our Podiatrist was able to complete the treatment for the first time in months without any concerns from the resident. Going forward, the resident’s son will be made aware of upcoming podiatry visits so he can be present to assist again.
This is a perfect example of the patience and communication required when working with individuals with dementia and complex needs. Our Podiatrist turned someone’s frustration into a positive outcome.
If you think a loved one can benefit from the assistance from our aged care and community Podiatrists, get in touch by clicking ‘Contact Us’ above or by giving us a call on 136 033.